I started looking at flare predication more closely with NASA's concern for a coming super solar flare..
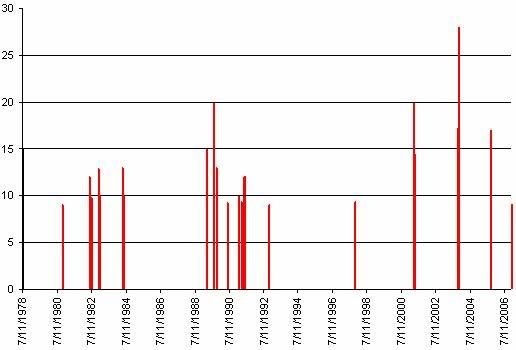
First I began with a listing of X-Class flares from 1975 forward…
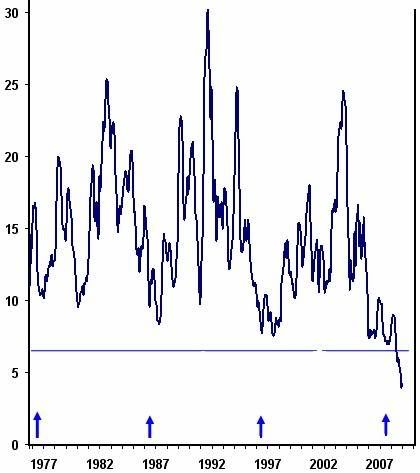
I then grabbed a five month averaged graph of the Ap Solar Progression for the same time period;
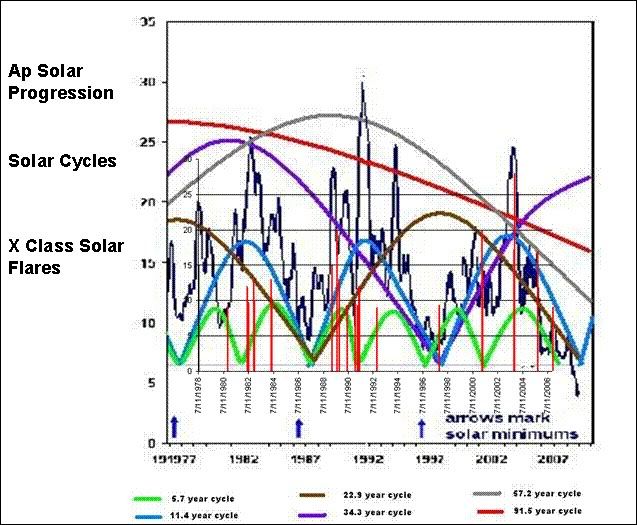
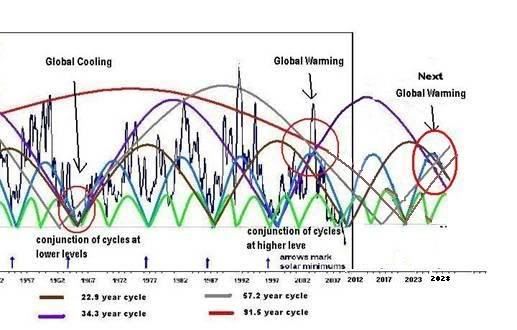
I overlaid these graphs with the six shortest solar cycles as I approximate them in length. It resulted in this…
The April 11th 2003 flare (ranking #1 – ~X28) is a good example of how large flares occur when multiple solar cycles converge.
It also can be seen easily in 1982 and 1984.
The predominance of flares in ~1991 seem tied to the peak of the ~67 year solar cycle maxima.
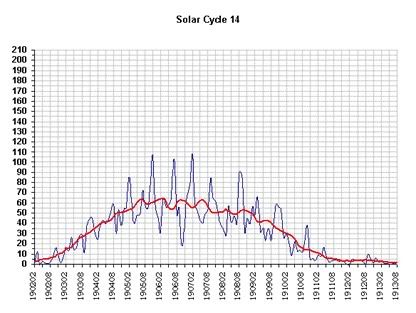
So if we look to the last Gleissberg minima of ~1905/06 and looked for X Class solar flares we should see some reflection of flares that lie ahead in the next Gleissberg minima.
It would appear that the date of last Gleissberg minima was the autumnal equinox of 1906.
In pushing my solar cycle/s theory into the future for an approximation of when the next higher level convergence will occur…
This is based on the Gleissberg minima occurring in solar cycle 25’s maxima
This should be prime time for solar flares.
This timing correlates with NASA’s window…
Solar flares appear predicatable as related to multiple solar cycles running concurrently and interacting with each other.
First I began with a listing of X-Class flares from 1975 forward…
Ranking Day/Month/Year X-Ray ClassProducing this graph;
----------------------------------------------
1 04/11/03 X28+
2 02/04/01 X20.0
2 16/08/89 X20.0
3 28/10/03 X17.2
4 07/09/05 X17
5 06/03/89 X15.0
5 11/07/78 X15.0
6 15/04/01 X14.4
7 24/04/84 X13.0
7 19/10/89 X13.0
8 15/12/82 X12.9
9 06/06/82 X12.0
9 01/06/91 X12.0
9 04/06/91 X12.0
9 06/06/91 X12.0
9 11/06/91 X12.0
9 15/06/91 X12.0
10 17/12/82 X10.1
10 20/05/84 X10.1
11 29/10/03 X10
11 25/01/91 X10.0
11 09/06/91 X10.0
12 09/07/82 X 9.8
12 29/09/89 X 9.8
13 22/03/91 X 9.4
13 06/11/97 X 9.4
14 24/05/90 X 9.3
15 05/12/06 X 9.0
15 06/11/80 X 9.0
15 02/11/92 X 9.0
I then grabbed a five month averaged graph of the Ap Solar Progression for the same time period;
I overlaid these graphs with the six shortest solar cycles as I approximate them in length. It resulted in this…
The April 11th 2003 flare (ranking #1 – ~X28) is a good example of how large flares occur when multiple solar cycles converge.
It also can be seen easily in 1982 and 1984.
The predominance of flares in ~1991 seem tied to the peak of the ~67 year solar cycle maxima.
Ranking Day/Month/Year X-Ray ClassThis just reinforces with me that solar flares are predictable when you correlate them to interactions between multiple solar cycles stumbling over each other.
----------------------------------------------
12 29/09/89 X 9.8
7 19/10/89 X13.0
14 24/05/90 X 9.3
11 25/01/91 X10.0
13 22/03/91 X 9.4
9 01/06/91 X12.0
9 04/06/91 X12.0
9 06/06/91 X12.0
9 11/06/91 X12.0
9 15/06/91 X12.0
11 09/06/91 X10.0
So if we look to the last Gleissberg minima of ~1905/06 and looked for X Class solar flares we should see some reflection of flares that lie ahead in the next Gleissberg minima.
It would appear that the date of last Gleissberg minima was the autumnal equinox of 1906.
In pushing my solar cycle/s theory into the future for an approximation of when the next higher level convergence will occur…
This is based on the Gleissberg minima occurring in solar cycle 25’s maxima
This should be prime time for solar flares.
This timing correlates with NASA’s window…
http://science.nasa.gov/science-news/science-at-nasa/2006/10may_longrange/
Long Range Solar Forecast
Solar flares appear predicatable as related to multiple solar cycles running concurrently and interacting with each other.